112 l © 2025 American Dental Association
Section 5: Cost
• In-school professionally applied topical fluoride
• In-school professionally applied dental sealants
• A control
After 4 years, approximately 50% of the original students were examined again. The study affirmed
the value and effectiveness of community water fluoridation. At the sites where the community water
was fluoridated, students had fewer cavities as compared to those sites without fluoridated water
where the same preventive measures were implemented. In addition, while sealants were determined
to be an effective prevention method, the cost of a sealant program was substantially more than
the cost of fluoridating the community water, reaffirming fluoridation as the most cost-effective
preventive option.478
In an effort to balance budgets, decision-makers sometimes make economic choices that amount to
being “penny wise and pound foolish.” In other words, they cut an expense today that appears to be a
sure money saver, but they fail to take a long-term view (or see the big picture) on the consequences
of that action. They fail to see how money spent now can provide greater savings in the future. A
decision to eliminate funding for a successful community water fluoridation program would be an
example of that kind of action.
Often, decision-makers are swayed by the promise of an alternative fluoride delivery system without
considering who it will cover (and who it will not cover), how it will be administered, and what it
will cost. Examples of these alternative fluoride delivery programs include school-based fluoride
mouthrinse programs, dietary fluoride supplements, fluoride varnish, and other professionally applied
topical fluorides. Often dental health education programs, including dispensing free toothbrushes and
fluoridated toothpaste, are mentioned as an alternative to fluoridation. All these programs can be
beneficial but are not as efficient or cost-effective as fluoridation programs because they typically
require additional personnel to facilitate the programs and action on the part of the recipient and have
much higher administrative and supply costs. Additionally, these programs typically target only children
and so do not provide decay-preventing benefits to adults. Fluoridation benefits all members of the
community— children and adults—and is more cost-effective.
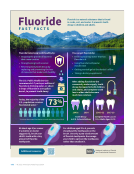
Health Impact in 5 Years Initiative
The CDC’s “Health Impact in 5 Years” (HI-5) initiative479 launched in 2016 highlighted community-wide
approaches that have evidence reporting (1) positive health impacts, (2) results in 5 years, and
(3) cost-effectiveness or cost savings over the lifetime of the population or earlier. Fluoridation is
one of the community approaches included in the HI-5 Initiative because it helps to keep people
healthy as it reaches all members of a community where they live, learn, work, and play.
Documenting the impact of fluoridation can be challenging, partially because the beneficial effect is
not immediately apparent.104 Cost savings from fluoridation would be expected to accumulate over
several years’ time. The most notable decrease in tooth decay would be anticipated in young children
who received the benefits of fluoridation over their lifetime in both their primary teeth and as their
adult teeth begin to appear when the children are approximately 6 years old.
Section 5: Cost
• In-school professionally applied topical fluoride
• In-school professionally applied dental sealants
• A control
After 4 years, approximately 50% of the original students were examined again. The study affirmed
the value and effectiveness of community water fluoridation. At the sites where the community water
was fluoridated, students had fewer cavities as compared to those sites without fluoridated water
where the same preventive measures were implemented. In addition, while sealants were determined
to be an effective prevention method, the cost of a sealant program was substantially more than
the cost of fluoridating the community water, reaffirming fluoridation as the most cost-effective
preventive option.478
In an effort to balance budgets, decision-makers sometimes make economic choices that amount to
being “penny wise and pound foolish.” In other words, they cut an expense today that appears to be a
sure money saver, but they fail to take a long-term view (or see the big picture) on the consequences
of that action. They fail to see how money spent now can provide greater savings in the future. A
decision to eliminate funding for a successful community water fluoridation program would be an
example of that kind of action.
Often, decision-makers are swayed by the promise of an alternative fluoride delivery system without
considering who it will cover (and who it will not cover), how it will be administered, and what it
will cost. Examples of these alternative fluoride delivery programs include school-based fluoride
mouthrinse programs, dietary fluoride supplements, fluoride varnish, and other professionally applied
topical fluorides. Often dental health education programs, including dispensing free toothbrushes and
fluoridated toothpaste, are mentioned as an alternative to fluoridation. All these programs can be
beneficial but are not as efficient or cost-effective as fluoridation programs because they typically
require additional personnel to facilitate the programs and action on the part of the recipient and have
much higher administrative and supply costs. Additionally, these programs typically target only children
and so do not provide decay-preventing benefits to adults. Fluoridation benefits all members of the
community— children and adults—and is more cost-effective.
Health Impact in 5 Years Initiative
The CDC’s “Health Impact in 5 Years” (HI-5) initiative479 launched in 2016 highlighted community-wide
approaches that have evidence reporting (1) positive health impacts, (2) results in 5 years, and
(3) cost-effectiveness or cost savings over the lifetime of the population or earlier. Fluoridation is
one of the community approaches included in the HI-5 Initiative because it helps to keep people
healthy as it reaches all members of a community where they live, learn, work, and play.
Documenting the impact of fluoridation can be challenging, partially because the beneficial effect is
not immediately apparent.104 Cost savings from fluoridation would be expected to accumulate over
several years’ time. The most notable decrease in tooth decay would be anticipated in young children
who received the benefits of fluoridation over their lifetime in both their primary teeth and as their
adult teeth begin to appear when the children are approximately 6 years old.